How Integrated Data Scales ABA Care — From Silos to Signals (Motivity Motivators Podcast)

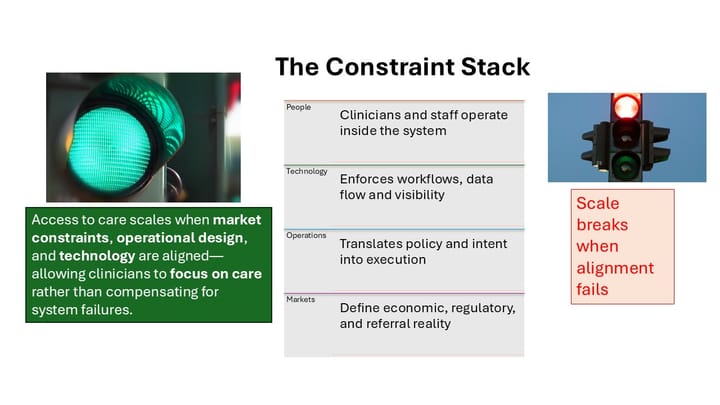
Why connecting PM/EHR with payroll, credentialing, incentives, and ATS turns data silos into decision signals that scale access and quality in ABA.
In Motivity’s Motivators Podcast, I joined CEO Smith Anderson and CCO Emaley McCulloch for a roundtable on the future of ABA operations and technology.
The conversation reinforced a point I see every day: ABA providers don’t lack data — they lack connected, actionable data. When practice management and EHR systems link with payroll, credentialing, incentives, and ATS, the shift is profound. Silos become signals, and leaders stop reacting to problems and start anticipating opportunities.
🎥 Watch the conversation
Key Takeaways
1. From Capture to Actionable Insight
It’s not enough to collect PM/EHR data. True leverage comes when it’s connected with payroll, credentialing, incentives, and onboarding systems.
“The shift is from data capture to decision enablement. Connect PM/EHR with payroll, credentialing, incentives—you finally see the whole operation.”
2. Ops & Clinical: One Feeds the Other
Operational efficiency is not at odds with clinical quality. In fact, it funds and protects it.
- Stronger retention
- Reduced burnout
- Resources to reinvest in care delivery
“Mission vs. margin is a false choice—operational health protects clinical quality.”
3. AI That Pays Off Now
The near-term wins are on the administrative side:
- Denial prediction
- Credentialing alerts
- Incentive alignment
- Staff attrition risk modeling
Most “AI” in market is still rules-based, but even that removes admin drag so clinicians can focus on care.
4. Proactive Decision Support
Reactive management is no longer sustainable. Providers need an enterprise decision layer—dashboards and alerts spanning clinical, RCM, compliance, and HR.
Think of it as Salesforce for ABA: data liquidity, open APIs, and ecosystem integrations.
5. Outcomes, Standards, and Scale
Scaling ABA long-term requires industry alignment on outcomes and standards. Value-based care is coming, and providers must be ready to measure and report consistently. Consolidation will favor platforms that expose data and integrate openly.
“The future doesn’t exist without scale. Rising tides raise all ships, and competition plus access to data will drive innovation.”
📌 Action Steps for Providers
- Unify your data: connect PM/EHR to payroll, credentialing, HRIS, and ATS.
- Define a small set of KPIs that mix clinical, RCM, and workforce health.
- Stand up early-warning signals (credential expirations, denial spikes, utilization dips).
- Pilot admin-side AI before clinical AI.
- Document standards for clinical quality and treatment efficiency.
Closing
The conversation with Smith and Emaley underscored that scaling ABA isn’t about choosing between mission and margin. It’s about using integrated data to reduce friction, empower clinicians, and expand access to quality care.
I’ll continue highlighting real-world examples in upcoming posts. If your organization is using integrated systems to differentiate and scale, I’d love to hear your story.