Who Actually Owns the Care Plan in Autism?
One of the least examined—but most consequential—realities in autism care is this:
Autism care operates without a single, continuous owner of the care plan.
This is not because the system lacks capable professionals.
👉 It is because responsibility is distributed across disciplines and roles that were never designed to integrate with one another over time.
The system functions—but it functions by absorbing friction rather than resolving it.
Autism Care Begins Fragmented—and Stays That Way
Autism care does not unfold inside a unified clinical model.
It unfolds across a sequence of handoffs, disciplines, and environments.
- Primary care physicians initiate referrals but rarely oversee care once services begin
- Diagnosticians assess, document, and exit—transactional by design
- Therapists deliver care within scoped plans but do not own longitudinal decisions
- Schools and home environments materially shape outcomes without formal alignment
- Operations teams manage constraints but do not own clinical intent
Each role behaves rationally within its mandate.
Collectively, the system lacks continuity.
What emerges is not coordinated care, but adjacent care: multiple actors touching the same child without a shared ownership model.
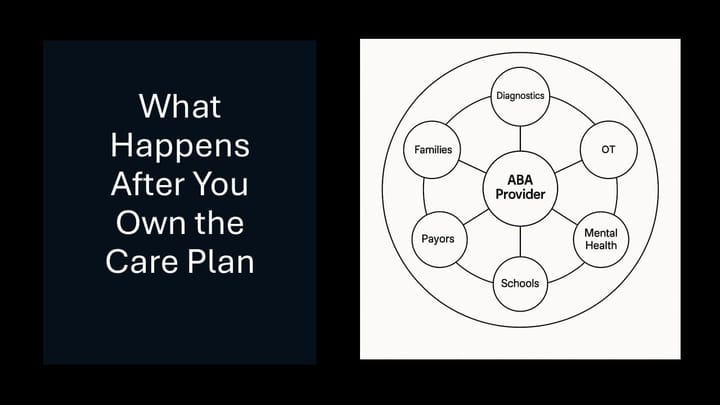
Adjacent Therapies Make the Ownership Gap Explicit
The fragmentation becomes even more visible when occupational therapy, speech therapy, and physical therapy enter the picture.
OT, ST, and PT are frequently part of a child’s care experience:
- Sometimes medically prescribed
- Sometimes school-based
- Sometimes delivered by entirely separate organizations
These therapies:
- Operate under different clinical frameworks
- Set goals independently
- Measure progress separately
- Rarely share a common planning or decision structure
They are not owned by ABA.
👉 And they are often not owned by anyone else either.
Autism care is multi-disciplinary—but not multi-integrated.
No discipline owns cross-discipline coherence.
How Ownership Quietly Collapses Into One Role
In the absence of a designed integrator, ownership does not disappear.
It concentrates.
Over time, responsibility lands with the only role that remains continuously engaged with the child’s functional progress: the BCBA.
Not because the role was architected to integrate the system—but because someone has to.
The BCBA as De Facto Quarterback
BCBAs are the closest thing autism care has to a quarterback.
They:
- Own the treatment plan
- Monitor progress over time
- Supervise therapists
- Are implicitly accountable for outcomes
They become the point where fragmented inputs—clinical, environmental, and operational—are reconciled into something coherent.
But this ownership emerges by default, not by design.
The Authority–Responsibility Mismatch at the Core of Autism Care
Once ownership collapses into the BCBA role, a structural problem becomes unavoidable.
BCBAs are responsible for outcomes—but do not control:
- Scheduling stability
- Staffing continuity
- Authorization timelines
- School cooperation
- Caregiver follow-through
- Cross-discipline handoffs
They are expected to adapt the care plan continuously in response to forces they cannot directly shape.
This is not failed leadership.
👉 It is a system asking one role to integrate what the system itself does not.
As organizations scale, this mismatch often compounds rather than resolves.
What Quietly Breaks as a Result
Accountability concentrates without authority.
Decision-making fragments while outcomes remain singular.
Clinical work is crowded out by exception management.
This is not inefficiency.
👉 It is cognitive overload embedded in the care model.
Where Broader Clinical Ownership Becomes Possible
There are emerging autism care models that attempt to solve this problem by centralizing clinical ownership above any single discipline—integrating ABA, medical care, parent training, and adjacent therapies under a unified care plan.
These models are often discussed in the context of value-based care, but their most important characteristic is not reimbursement structure.
It is design discipline.
They require:
- Explicit authority to interpret outcomes across settings
- Longitudinal definitions of progress
- Shared data infrastructure across disciplines
- Organizational commitment to integration, not just collaboration
They are difficult to build, slow to scale, and currently the exception rather than the norm.
But they demonstrate something important:
When clinical ownership is truly centralized and outcomes are defined longitudinally, the integration burden no longer collapses entirely onto the BCBA. It moves into the system itself.
This does not eliminate the BCBA’s role as clinical center of gravity.
It changes the conditions under which that role operates.
What a Path Forward Actually Requires
This problem does not require ABA to absorb more responsibility.
It requires designing honestly around how ownership already emerges—and redistributing integration work accordingly.
- Clinical ownership must be singular and explicit
Whether it sits with a BCBA today or a broader integrator role in the future, ownership cannot be distributed without authority. - Clinical integration must be separated from operational coordination
One role cannot sustainably carry both. - Cross-discipline coordination must become a first-class capability
Multi-disciplinary care without integration is not coordination—it is adjacency.
These are design requirements, not feature requests.