Credentialing in ABA: Navigating the Lifecycle, Systems, and Stakeholders
Credentialing in ABA is more than just paperwork—it’s a high-stakes operational function that directly impacts compliance, billing eligibility, and payor alignment. Whether you're a growing provider managing hundreds of clinicians or a nonprofit coordinating subcontracted teams, credentialing touches nearly every part of the care delivery and revenue cycle.
Yet the systems and workflows to manage credentialing remain fragmented. Some providers lean on HRIS platforms. Others depend on CAQH, spreadsheets, or custom automations. A few emerging tools are now trying to bring order to this complexity—but adoption is still early.
In this post, we’ll map out:
- The full credentialing lifecycle
- How providers operationalize credentialing
- Key vendors and tools (both in use and emerging)
- The role of nonprofits and subcontractors
- Credentialing authorities and industry standards
🧭 The Credentialing Lifecycle in ABA
Credentialing isn’t a one-time task—it’s an ongoing operational cycle. Key stages include:
- Define Required Credentials
Based on service lines, payor contracts, roles (e.g., RBT, BCBA), and state/federal regs. Clinical, HR, and Compliance teams typically collaborate here. - Assign and Track
Internal teams map credentials to job roles and determine what’s needed for each employee: CPR, supervision hours, CEUs, background checks, NPI, etc. - Acquire and Maintain
Staff must complete trainings, submit documents, and track hours. CEU renewal cycles and supervision thresholds need continual monitoring. - Verify and Store
Credential documents must be verified, stored securely, and made accessible for audits or payor onboarding. Internal QC checks are common. - Payor Credentialing and Alignment
Credentialed staff must be registered with payors—either directly or through intermediaries like CAQH. Their credential status must align with session billing logic. - Ongoing Compliance and Audits
Expiring licenses, CEUs, and recredentialing events must be proactively tracked. Some orgs embed alerts or automate offboarding workflows tied to lapses.
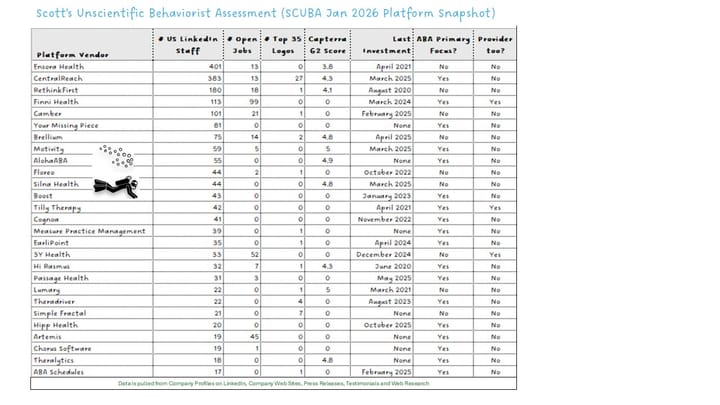
🧰 Credentialing Tools & Platforms in ABA
Credentialing tools fall into four categories: production-ready platforms, emerging tools, custom workflow systems, and required infrastructure.
✅ Actively Used in ABA Credentialing Workflows
| Vendor | Category | Use Case | Notes |
|---|---|---|---|
| CentralReach | PM Platform | Tracks certifications, CEUs, expirations; links credentials to payors | Widely used among large ABA orgs; credentialing tied to employee records and billing |
| Lumary | PM Platform (Salesforce-based) | Credential tracking integrated with onboarding, compliance, and HRIS | Flexible Salesforce objects support complex workflows, including payor alignment |
| Artemis | PM Platform | Tracks credential-payor alignment for scheduling and billing | Emphasizes compliance-linked ops workflows; used by scaled multi-site providers |
| Gusto / ADP / Paylocity | HCM / HRIS | Tracks licenses, expirations, CEUs | Not ABA-specific; common for internal compliance and reminders |
| Relias | CEU / Training | Offers RBT/BCBA training, CEU tracking | Used for onboarding and continuing education; not a full credentialing tool |
| MentraTrack | Supervision & Credential Tracking | Tracks RBT and BCBA supervision hours, compliance, and documentation | Purpose-built tool for supervision tracking and pre-certification credentialing |
🟧 Emerging or Limited-Use Tools (As of Mid-2025)
| Vendor | Category | Use Case | Notes |
|---|---|---|---|
| Clinivise | Credentialing / Compliance | Building credential tracking and supervision hour tools | In development; early CEU/supervision tracking features but no confirmed production use yet |
| Medallion / Verifiable | Credentialing APIs | License verification, payor enrollment (used in broader healthcare) | Limited or no adoption in ABA as of mid-2025 |
| Certemy | License Compliance | Workflow automation for license and CEU verification | Some healthcare presence, but not known in ABA-specific implementations |
🟨 Workflow Tools for Custom Credentialing Management
| Vendor | Category | Use Case | Notes |
|---|---|---|---|
| Airtable / Monday.com / Zoho | Automation / Workflow | Commonly used to build custom credential tracking tools | Not plug-and-play; flexible for internal ops teams |
| Simple Fractal | Automation Services | Used for custom integrations and automation in credentialing or onboarding | No out-of-the-box product; project-based automation for larger orgs |
🏛️ Credentialing Infrastructure & Required Databases
| Entity | Function | Use Case | Notes |
|---|---|---|---|
| CAQH | Credentialing Clearinghouse | Payor enrollment for BCBAs and licensed clinicians | Common clearinghouse, though not ABA-specific |
| PECOS / NPPES | Federal Provider Databases | NPI registration and Medicare enrollment | Essential for providers working with federal or Medicaid plans |
| BACB | Credentialing Authority | Governs and verifies BCBA, BCaBA, and RBT credentials | Source of truth for credential validity and supervision auditing |
🧑🤝🧑 Nonprofits & Subcontractor Credentialing
Many large nonprofits (e.g., Merakey, Elwyn, Vinfen, Bancroft) play a unique role in the credentialing ecosystem:
- Dual Models: Some deliver ABA services directly and subcontract to other providers or solo practitioners.
- Credential Aggregation: Must validate and track external credentials from partner agencies.
- Audit Burden: Require full documentation and often run internal audits to ensure partner staff meet payor requirements.
- Technology Challenges: Most use a patchwork of HCM tools, shared drives, or custom tracking systems—highlighting a gap in nonprofit-aligned credentialing infrastructure.
This layer of coordination is often overlooked in platform development, despite being essential to maintaining care delivery at scale.
🧩 Organizational Accreditation & Industry Standards
Credentialing isn’t shaped by platforms alone. Two key organizations influence how ABA providers structure their credentialing systems:
🏥 Jade Health (formerly BHCOE)
- Offers outsourced credentialing and contracting services for ABA providers.
- Helps organizations prepare and submit credentialing documents to payors, manage recredentialing timelines, and ensure clinician files are audit-ready.
- Operates alongside their accreditation services, offering a combined compliance and operational value proposition for growing providers.
🧭 Council of Autism Service Providers (CASP)
- Publishes practice guidelines that include staffing, supervision, and credentialing expectations.
- Hosts webinars and policy briefs on topics like delegated credentialing and multi-site credential alignment.
- While not a credentialing vendor, CASP’s standards shape how many providers define internal credentialing and compliance structures.
These organizations help formalize credentialing expectations in the absence of federal uniformity—especially important as the ABA field continues to mature.
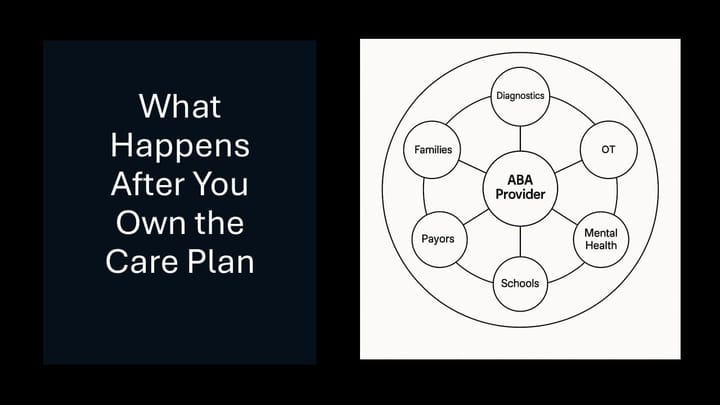
📈 Credentialing as a Strategic Lever
Credentialing isn’t just compliance—it’s operational leverage. The best-run ABA providers use credentialing data to:
- Speed Onboarding: Reduce delays in seeing clients by pre-clearing staff for credential alignment
- Optimize Staffing: Route credentialed staff to contracts that require specific qualifications
- Ensure Billing Accuracy: Avoid denied claims tied to credential mismatches
- Support Quality and Access: Align clinician qualifications to learner needs and payor standards
As the ABA space matures and consolidates, we expect more purpose-built platforms to emerge. Until then, providers must blend off-the-shelf tools, credentialing authorities, and internal processes to stay ahead of payor and audit requirements.