From Referral to Treatment: Fixing the Diagnostic Bottleneck in ABA
In ABA, nothing starts without a diagnosis.
For families, it’s the ticket to services.
For payors, it’s the proof of medical necessity.
And for providers, it’s the first step in a relationship that can last years.
Yet in 2025, the diagnostic process is still a bottleneck — one that delays care, frustrates caregivers, and costs providers revenue. The good news? With the right workflows, partnerships, and technology, it doesn’t have to be.
Why Diagnostics Matter
Insurers require a qualifying diagnosis before authorizing ABA services. That evaluation, whether done by a developmental pediatrician, psychologist, or a validated digital tool, is the cornerstone for:
- Establishing medical necessity
- Aligning treatment with clinical guidelines
- Tracking outcomes that matter to payors
Just as importantly, diagnostics don’t always lead to ABA — and that’s a good thing. A thorough evaluation can:
- Confirm the need for autism-specific therapy and open the door to ABA services.
- Identify co-occurring conditions (e.g., speech delays, sensory processing issues, ADHD) that can be treated in parallel or even addressed first for better outcomes.
- Redirect families toward alternative services when autism isn’t the underlying diagnosis, preventing unnecessary waitlist time and ensuring a child gets the right intervention earlier.
Without this clarity, treatment plans risk being delayed, misaligned, or ineffective — no matter how ready the provider is to start.
How Referrals Flow
Referrals go both ways in the ABA ecosystem:
Inbound to ABA Providers
- Physicians and pediatric practices
- School districts and early intervention programs
- Advocacy groups and non-profits
- Parent self-referrals (often after online research or peer recommendation)
Outbound from ABA Providers
- To diagnosticians for families without a qualifying evaluation
- To specialists for co-occurring conditions (speech, OT, developmental medicine)
- To community clinics for uninsured or underinsured families
The friction points are predictable: incomplete paperwork, mismatched insurance coverage, missed follow-ups. Each one extends the time between initial inquiry and the start of therapy.
The Role of Non-Profits
Community-based organizations often sit at the center of referral networks. They:
- Educate families about autism signs and the need for evaluation
- Provide low/no-cost diagnostics for underserved populations
- Maintain close ties with both school systems and private providers
For ABA organizations, partnering with these non-profits can open access to families earlier in the care journey — and can be a powerful brand-building move.
The Caregiver Experience
For parents and caregivers, the diagnostic journey is rarely linear. Common pain points include:
- Long waitlists — sometimes 6–12 months
- Unclear insurance acceptance
- Limited availability of local specialists
- Uncertainty about what type of provider can issue an “accepted” diagnosis
Families often navigate this in an emotional fog, making clear communication and consistent follow-up critical.
Fixing the Process with Workflow + CRM
A well-structured referral workflow, supported by a capable CRM platform, can dramatically shorten diagnosis-to-treatment timelines — but only if it’s built to serve three key stakeholders at once:
- The ABA provider — intake teams, schedulers, and clinical leadership.
- The diagnosticians — whether in-house or external.
- The family — parents, caregivers, and sometimes school or Early Intervention coordinators.
Key Moves That Drive Impact
- Centralized Intake Tracking
Every referral — inbound or outbound — is entered into the CRM the moment it’s received, with fields for referral source, insurance, and next required step. This creates a single source of truth accessible to all authorized staff. - Automated, Role-Specific Reminders
- Intake coordinators get alerts to follow up on missing documents.
- Diagnostic schedulers receive prompts when evaluations haven’t been booked within a set timeframe.
- Clinical directors get notified if a family has been “stuck” in the diagnostic stage beyond a KPI target.
- Integrated Insurance Verification
Verification is triggered as soon as a diagnostic appointment is being scheduled. The CRM can push the request to the RCM/billing team, track completion, and flag denials or mismatches before they delay treatment. - Family-Facing Communication
Automated SMS or email updates confirm appointments, send document checklists, and remind families of prep steps (e.g., bringing school records or past assessments). These touchpoints reduce no-shows and incomplete evaluations. - Diagnostic Provider Coordination
For external diagnosticians, the CRM can:- Securely share intake packets and background information.
- Track when the evaluation report is received.
- Automatically update the ABA team when the report is uploaded so the treatment authorization process starts immediately.
- Post-Diagnosis Triggers
The moment a diagnosis is entered into the CRM, it can:- Alert scheduling teams to start treatment setup.
- Launch authorization requests with pre-filled diagnostic data.
- Notify clinical staff to draft treatment plans.
Why It Matters
Without a CRM-driven workflow, the diagnostic process becomes a game of phone tag and spreadsheet roulette. With one, every handoff — from intake to insurance to scheduling to clinical — is logged, tracked, and visible, reducing the chance of delays and improving the family’s experience at every stage.
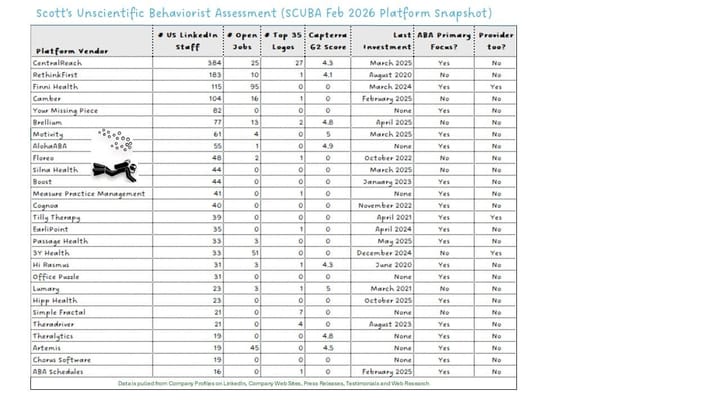
Emerging Tools: Cognoa, EarliTec, and Beyond
New digital diagnostic solutions are closing the gap between concern and confirmed diagnosis:
- EarliTec — video-based assessment tool with strong evidence for accuracy and speed.
- Cognoa — AI-assisted platform that can be used by PCPs to accelerate diagnosis.
Beyond just selling software, some of these companies are building networks of physicians trained and equipped to use their tools. The goal:
- Broader adoption — standardizing diagnostic protocols across multiple practices and states.
- Access expansion — connecting families to qualified diagnosticians, even in regions with long waitlists or few specialists.
- Enable efficiencies — with a more effective screening tool and process, physicians can more effectively manage their caseloads.
- Payor credibility — demonstrating scale and consistency to strengthen insurance acceptance.
In some cases, this physician-network approach transforms the tool into a turnkey referral solution — not just a piece of tech, but an entry point into a coordinated diagnostic pathway that providers can tap into directly.
When paired with a provider’s CRM-driven follow-up workflow, these networks have the potential to shrink diagnosis timelines from months to weeks, and to bridge access gaps in rural or underserved markets.
Risks and Considerations
- Variable payor acceptance — not all insurers will approve services based on a newer diagnostic method, especially if they are unfamiliar with the tool’s validation.
- Integration gaps — the diagnostic report may not flow cleanly into the provider’s EHR/PM system, creating manual work.
- Dependency risk — over-reliance on a third-party network can create delays or service gaps if the vendor changes pricing, availability, or coverage areas.
- Physician engagement — sustaining a high-quality diagnostic network requires ongoing training, incentives, and quality assurance.
Why Some Providers Bring Diagnostics In-House
For many ABA providers, the wait for an external diagnosis is the single biggest barrier to starting therapy. Bringing diagnosticians onto the payroll — developmental pediatricians, psychologists, nurse practitioners — is a direct way to control that bottleneck.
Pros
- Faster treatment starts — reduces lag from months to weeks or even days.
- Control over quality — consistent documentation aligned with payor requirements.
- Stronger parent experience — families have a single point of contact from screening to treatment.
- Data continuity — diagnostic findings flow directly into the treatment plan.
Cons
- High fixed costs — salaries, benefits, and overhead for specialized clinicians.
- Regulatory complexity — state-specific licensing and supervision requirements.
- Potential payor pushback — some insurers scrutinize diagnoses from providers who also deliver treatment, citing conflict-of-interest concerns.
- Capacity management — if diagnostic demand exceeds staff bandwidth, delays return.
- Geographic limitations — for providers with a wide service area, families may have to travel hours for an in-person diagnostic appointment.
The takeaway: In-house diagnostics can be a powerful competitive advantage, but only if they’re adequately staffed, payor-compliant, and operationally integrated into the broader intake process — and if travel time for families is realistically addressed.
Data as a Competitive Advantage
Forward-thinking ABA providers are treating diagnostic speed as a KPI:
- Time from initial inquiry to completed diagnosis
- Conversion rates by referral source
- Payor approval rates by diagnostic pathway
Over time, this data supports stronger payor negotiations — and positions the provider as an operationally efficient partner.
Where This is Headed
In-house diagnostics will remain the gold standard for speed and control, but even providers without that capacity can compete by:
- Building strong referral relationships
- Investing in CRM-driven intake workflows
- Adopting emerging diagnostic tools strategically
- Partnering with non-profits to broaden their reach
The winners won’t just be the providers who diagnose fastest — they’ll be the ones who make the process clear, connected, and caregiver-friendly.
If you run intake, operations, or strategy for an ABA provider, the question isn’t whether to improve your diagnostic process. It’s how soon you can make it a competitive edge.
Click here to subscribe for more insights on ABA technology, operations, and strategy.