📬MissionViewpoint Monthly Update – February 2026

The Mission of MissionViewpoint
👉 To drive more—and better—access to autism care through the smarter use of technology and data.
Credo
This is the twelfth consecutive monthly edition of MissionViewpoint.
After a year of observing autism care operating at scale, one constraint has become explicit.
MissionViewpoint only promotes, participates in, or aligns with work that plausibly leverages technology, operations, or data to expand access to autism care without degrading quality.
That constraint governs what is written, who is engaged, and which opportunities are declined. It is not an editorial posture. It is an operating rule.
Welcome to the ABA Mission Viewpoint February 2026 Monthly Update
Theme: Second-Order Effects
January exposes pressure.
February reveals consequences.
Not the obvious ones—but the downstream effects of decisions that were reasonable, well-intentioned, and often necessary at the time they were made.
Autism care is a uniquely complex business. Care is delivered across fragmented clinical roles, disciplines, and environments. Pediatricians initiate care but rarely oversee it longitudinally. Diagnosticians assess and exit. OT, ST, PT, mental health services, schools, and home environments all influence outcomes without shared accountability. Workforce constraints and reimbursement pressure magnify every handoff.
As organizations scale, these dynamics do not disappear. They compound.
February is where those second-order effects become visible—when systems are technically working, but friction quietly accumulates.
That question—what breaks after things start working—is the throughline of this issue.
🧩 Who Actually Owns the Care Plan in Autism
Under pressure, familiar assumptions resurface. Autism care is often described as multidisciplinary and collaborative—but that framing obscures a structural reality: there is rarely a single, continuous owner of the care plan.
Each role behaves rationally within scope. Pediatricians refer. Diagnosticians document. Therapists deliver scoped services. Schools and families operate under independent constraints. Operations teams manage capacity and compliance.
Responsibility does not disappear. It concentrates.
Over time, accountability collapses onto the one role continuously closest to functional progress: the BCBA. Not because the role was designed to integrate the system—but because someone has to.
As organizations scale, this authority–responsibility mismatch compounds. Clinical judgment is increasingly crowded out by exception management. Coordination becomes implicit rather than designed.
Takeaway:
Autism care does not lack capable professionals. It lacks a designed owner of longitudinal coordination—and second-order strain emerges where ownership is assumed rather than architected.
🧠 What Happens When ABA Providers Become Care Organizations
Many ABA providers are expanding beyond clinic-based therapy into diagnostics, OT, ST, mental health services, school coordination, and broader care offerings.
At the first order, these moves make sense. They reduce care leakage, improve the family experience, and align with whole-child care narratives.
The second-order effects are harder to see.
As scope expands, responsibility grows faster than control.
- Leadership shifts from therapy oversight to system orchestration.
- Productivity metrics strain under cross-discipline reality.
- Intake efficiency creates downstream scheduling fragility.
- “Comprehensive care” increases coordination surface area without matching reimbursement models.
Growth quietly becomes a risk-transfer exercise.
Takeaway:
Scope expansion is not just capability expansion. It is failure-surface expansion—and organizational design determines whether that risk compounds or stabilizes.
🤖 The Hidden Cost of Building Your Own Stack in the Age of AI
AI has lowered the cost of writing software. It has not lowered the cost of operating it inside a healthcare delivery organization.
Providers evaluating build-versus-buy decisions often focus on speed, flexibility, and avoiding vendor constraints. What receives less attention is orchestration load:
- unstable requirements across states and payors,
- testing and maintenance discipline, model drift, and
- staff quietly becoming product managers and QA teams.
In autism care, those costs compound quickly.
A small number of providers may successfully build defensible internal systems. Most will realize more value by delegating AI complexity to vendors —while reserving internal investment for narrow, justified differentiators.
Takeaway:
The scarce resource is not AI capability. It is orchestration capacity—and underestimating it creates second-order risk.
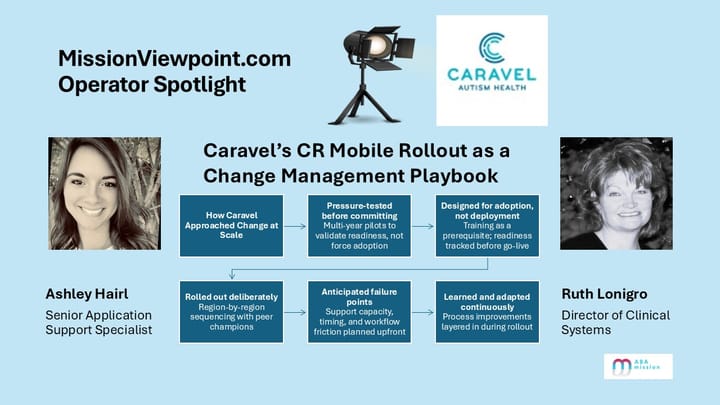
💡 Operator Spotlight: Caravel Autism Health
Periods of change often push stress downstream. New tools are deployed quickly, adoption is forced, and frontline teams must absorb the consequences.
Caravel Autism Health took a different approach with its CR Mobile rollout.
Rather than rushing deployment, the organization pressure-tested reality through extended pilots. Training was treated as a prerequisite, not a recovery step. Support was designed to scale without burning out staff. Constraints were allowed to surface broken processes—and then used as prompts to fix them.
Several second-order benefits followed: improved amendment workflows, earlier detection of authorization and coding issues, and stronger links between documentation and timesheets.
Takeaway:
The scalable advantage is not adopting technology. It is building repeatable change discipline that contains disruption instead of exporting it to clinicians and families.
✅ Platform Highlights
- Viventium acquired Apploi, combining payroll, compliance, and workforce acquisition into a more vertically integrated human capital platform for healthcare providers.
Why it matters: labor infrastructure is becoming a control point for scale and margin in autism care. A deeper look at platform consolidation next month. - Brellium partnered with Anthropic to support Claude for Healthcare in chart review and documentation workflows.
- Silna Health launched Predictive Document Intelligence for prior authorization validation.
- Catalight partnered with Frontera Health to expand access to AI-enabled assessment and care tools.
- AlohaABA released a new TheraDriver integration.
- TheraDriver added ACES as a top 35 customer.
- CASP acquired Jade Health (including BHCOE), consolidating accreditation under ACQ.
- AnswersNow raised $40M in Series B funding.
Takeaway:
This month’s platform activity reflects execution surfacing—not repositioning.
📊 Provider Trends
- Payor pressure continues to land in operational mechanics rather than headline rate action.
- A mid-tier cohort outside the Top 20 remains disproportionately strong on visible momentum.
- Service-mix strategies are diverging by scale. Smaller and mid-sized providers (e.g., KidsChoice) continue expanding OT and ST to deepen care and referrals, while larger platforms (e.g., ACES) are simplifying and unwinding in-house ancillary services as coordination costs rise.
- Hiring remains selective and role-specific rather than broadly re-accelerating.
Takeaway:
The market isn’t pausing. It’s revealing the downstream impact of choices already made.
💬 Closing Thoughts
Second-order effects are what separate growth from resilience.
In autism care, systems rarely fail because they are broken. They fail because they are working inside a care model that compounds complexity—fragmented ownership, multi-environment delivery, workforce volatility, and payor enforcement that punishes ambiguity.
February is where those consequences surface.
The organizations that expand access without degrading quality will not be defined by scale alone, but by their ability to recognize second-order failure modes early—and design around them deliberately.
Until next time,
— Scott
P.S. Know someone shaping ABA operations, technology, or investment? Invite them to subscribe at missionviewpoint.com.
In March: Why Autism Care Is Ripe for Consolidation—and Why It Keeps Failing.