The Invisible Layer in ABA Delivery: Behavioral Health Management Organizations
When we talk about access to ABA therapy, most people think about two players:
the payor (insurance company or Medicaid plan) and the provider (the ABA organization delivering care).
But in many markets, there’s a third, often invisible layer that determines how and when therapy actually happens:
Behavioral Health Management Organizations — the entities that sit between payors and providers, managing networks, authorizations, and data.
What These Organizations Do
Behavioral health management organizations (BH-MOs) act as administrative and clinical intermediaries for health plans.
They exist because managing behavioral health benefits—especially ABA—requires a level of specialization most payors don’t maintain internally.
Their core functions include:
- Network management: recruiting, credentialing, and contracting providers.
- Utilization management: reviewing authorizations, treatment plans, and progress reports.
- Care coordination: helping families navigate eligibility, referrals, and ongoing service changes.
- Compliance and data reporting: aggregating encounter data and outcomes to satisfy plan or state requirements.
In short, BH-MOs translate insurance benefits into operational rules for real-world providers.
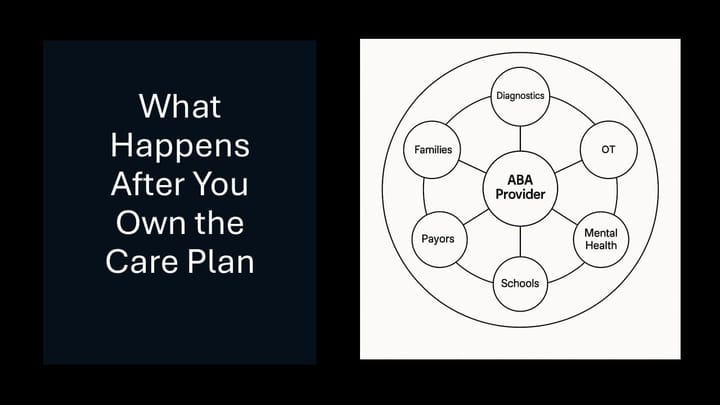
How They Fit into the ABA Ecosystem
Here’s a simplified view of the delivery chain:
Government or Commercial Payor → Behavioral Health Management Organization → ABA Provider → Family
- The payor defines and funds the benefit.
- The BH-MO administers that benefit—setting policies, processing authorizations, and maintaining compliance.
- The provider delivers services and navigates those administrative requirements.
- The family experiences the outcome—how quickly care begins, how long it continues, and how consistent it feels.
This structure can make access feel fragmented: families see the insurance logo, but operational control sits elsewhere.
How Providers Work with BH-MOs
For most ABA companies, the relationship follows a common pattern.
1. Network Contracting
Providers enroll through the BH-MO’s credentialing system, often separately from the underlying insurance network.
Contracts define rates, covered services, and documentation standards that may differ from the payor’s standard terms.
2. Referral and Assignment
Referrals can originate from families, physicians, or case managers.
The BH-MO verifies eligibility, confirms benefit design, and routes cases to in-network providers based on geography, capacity, and network adequacy rules.
That’s why directory accuracy, response time, and capacity reporting directly affect referral flow.
3. Authorization and Ongoing Review
Providers submit initial assessments and treatment plans through the BH-MO’s portal or form library.
These are reviewed by clinicians—often BCBAs—who ensure the plan aligns with policy and medical-necessity guidelines.
Re-authorizations occur at defined intervals, with updated goals and progress summaries.
This rhythm—intake, authorization, service, re-auth—is universal, but every BH-MO layers its own cadence, forms, and documentation rules.
Why Payors Use Them
From the payor’s perspective, behavioral health management is high-friction work.
It requires clinical expertise, regulatory knowledge, and real-time case oversight—none of which scale easily inside a traditional health plan.
By delegating to a BH-MO, payors can:
- Offload utilization management and network oversight while retaining financial control.
- Reduce compliance risk for behavioral benefits.
- Satisfy state Medicaid carve-out requirements through specialized contractors.
- Maintain data pipelines for cost and quality reporting.
The result is a distributed but controlled model—outsourced administration with payor-level accountability.
How Referrals and Service Assignments Work
Referrals typically follow one of three paths:
- Parent or PCP → BH-MO
The family or clinician calls the number on the back of the insurance card. The BH-MO confirms eligibility, screens for network availability, and assigns an in-network provider. - Provider → BH-MO
The ABA organization verifies that the member’s benefit is managed by a BH-MO, then uploads intake documentation for authorization. - State Agency → BH-MO (Medicaid ASO model)
In some states, the BH-MO acts as the access line for public autism benefits—matching families to contracted providers or regional centers.
Regardless of route, the BH-MO becomes the gatekeeper for authorization and care continuity.
The Competitive Landscape
Behavioral health management organizations vary in ownership and orientation, but a handful dominate the market across commercial and government contracts.
- Carelon Behavioral Health (formerly Beacon, part of Elevance Health) remains the largest delegated administrator in autism and behavioral health.
- Optum Behavioral Health (UnitedHealth Group) runs one of the most vertically integrated ecosystems, pairing its payor, data, and provider arms.
- Magellan Healthcare (now part of Centene) continues to manage Medicaid carve-outs and state behavioral programs.
- Lucet (formerly New Directions Behavioral Health + Tridiuum) focuses on access management and digital screening, often sitting between payors and regional provider networks.
- PerformCare (AmeriHealth Caritas) and other public-sector ASOs like Value Behavioral Health of Pennsylvania or Partners Health Management remain critical in Medicaid and children’s behavioral carve-outs.
- Two integrated insurers also operate as BH-MOs within their own plans:
Evernorth Behavioral Health (Cigna) and Aetna Behavioral Health, both of which manage utilization review, network access, and outcomes reporting directly for their covered populations.
Together, these organizations form the administrative backbone of behavioral health delivery — competing less on brand than on efficiency, compliance, and data transparency.
Families may never know their names, but their processes define how ABA therapy actually begins.
🔭 Evolving Access Models
A few emerging companies are reimagining how families find and engage with autism and neurodiversity services — without taking on the full administrative role of a behavioral health management organization.
- Lyra Health and Spring Health are expanding their employer-based behavioral platforms to include neurodiversity and family programs, offering diagnostic evaluations, caregiver coaching, and care navigation.
- RethinkCare, part of RethinkFirst, remains one of the most autism-specific entrants — providing BCBA-led caregiver support and workplace neurodiversity education at enterprise scale.
While these models don’t manage payor authorizations or claims, they share the BH-MO goal of improving access and coordination. For ABA providers, they represent a growing referral and caregiver-engagement layer at the front door of the autism-care ecosystem.
How Tech, Ops, and Data Strengthen Provider Relationships with BH-MOs
Behavioral health management organizations are slow to modernize—but providers don’t have to wait for them.
The most efficient ABA companies use technology to standardize, operations to streamline, and data to influence.
Here’s what that looks like in practice:
- Technology: Build structured intake and billing workflows that automatically align with each BH-MO’s forms, required fields, and re-auth cadence. Even basic automation—like auto-generating prefilled authorization packets or flagging expiring authorizations—can cut admin time by 30–50%.
- Operations: Treat each BH-MO like its own market. Document their rules, contact points, and timelines in one shared playbook, and train staff to follow it consistently. A clear handoff process between intake, clinical, and billing teams eliminates the bottlenecks BH-MOs often amplify.
- Data: Track the cycle time between referral, authorization, and first session. Then monitor denial rates and re-auth turnaround times by BH-MO. These metrics create leverage in contract discussions and identify where operational fixes pay off fastest.
Every pre-auth, progress report, and claim is a data point.
When structured and analyzed, that information becomes more than compliance—it’s your evidence of reliability, efficiency, and quality, which are the exact levers BH-MOs (and payors) respond to.
Building a Tech Stack That Can Handle Behavioral Health Management Organizations
Working with BH-MOs isn’t just a clinical or billing challenge—it’s an enterprise integration challenge.
Each BH-MO enforces its own rules, file formats, and documentation cadence.
To stay efficient, providers need systems that can absorb that complexity without overwhelming staff.
1. A Configurable Practice Management Core
Your core platform should support:
- Multiple payor and authorization structures.
- Dynamic treatment-plan templates that adjust to BH-MO fields.
- Audit-ready, versioned documentation.
Rigid platforms collapse under this variability; flexible ones scale with it.
2. Integrated Intake and Authorization Workflows
Create structured workflows that make compliance automatic:
- CRM-driven checklists triggered by plan and market.
- Automated packet generation (prefilled forms, attachments, e-signature routing).
- Dashboards tracking pending, expiring, and denied authorizations.
The objective: make re-auth compliance routine, not reactive.
3. Billing and Claims Automation
Clean claims are the bridge between provider and BH-MO:
- Claims scrubbing for behavioral codes and modifiers.
- Automated eligibility checks and rules-based billing by contract logic.
- Exception handling workflows for partial payments and re-bills.
Billing automation keeps BH-MO friction from becoming a cashflow crisis.
4. Data Warehouse or Analytics Layer
BH-MOs report on compliance and cost; providers can report on access and outcomes.
- Track authorization-to-claim lag and denial reasons.
- Benchmark utilization by BH-MO or plan.
- Visualize where administrative friction is highest.
- Build payor scorecards for negotiations and performance reviews.
5. Secure Integration & API Strategy
Even if a BH-MO still runs on portals, prepare for the future:
- Support FHIR, HL7, or JSON-based data exchange.
- Use RPA or middleware for interim automation.
- Maintain strong data governance and HIPAA compliance.
- Enable event-driven workflows like “auth approved → scheduler notified.”
Integration readiness today prevents tech debt tomorrow.
6. Operational Command Layer
Technology only delivers if paired with operational ownership:
- A dedicated Payor Operations team to manage BH-MO relationships.
- System admins who maintain mapping, forms, and rules.
- Feedback loops between intake, clinical, and billing teams.
Strong systems need strong stewards.
The Bigger Picture
Behavioral health management organizations will continue to shape how ABA care is authorized, delivered, and measured.
The providers who succeed won’t be those who complain about complexity—they’ll be the ones who instrument it:
capturing the right data, automating the right workflows, and using insight to turn administrative friction into operational edge.
The invisible layer is here to stay.
The question is whether your systems—and your strategy—are built to work with it.
👉 Subscribe to the ABA Mission Newsletter for regular insights into ABA strategy, tech platforms, and investment activity.
🔗 Sign up here